Abdominal aortic aneurysm
Jan 06, 2025Abdominal aortic aneurysm refers to an aneurysm-like expansion of the abdominal aorta. An aneurysm is usually defined as an increase in diameter of more than 50%. Most patients with abdominal aortic aneurysm are asymptomatic and are often discovered incidentally during physical examination for other reasons. A small number of patients have compression symptoms, and upper abdominal fullness and discomfort are common.
If the aneurysm invades the lumbar spine, there may be lumbosacral pain. If severe pain in the abdomen or waist occurs recently, it often indicates that the tumor is on the verge of rupture. Patients with acute rupture present with sudden severe pain in the lower back, accompanied by shock.
Abdominal aortic aneurysm resection originated from the early exploration of aneurysm surgery, and after continuous development and improvement, it has gradually formed two main methods of modern laparotomy and endovascular treatment.
Open abdominal aortic aneurysm repair
Abdominal aortic aneurysm resection and artificial blood vessel transplantation originated in the 1960s. After more than half a century of development, they have continued to evolve and mature, and have become one of the classic vascular surgery operations.
Surgical risks should be fully assessed before surgery. Cardiovascular events are an important cause of death after abdominal aortic aneurysm repair.Cardiac evaluation can be performed on high-risk patients. Patients who are elderly or have a history of stroke should routinely undergo carotid artery Doppler examination to understand the condition of the carotid arteries.For patients with rupture, the above-mentioned examinations should be completed as much as possible before surgery, but life-saving is the primary criterion.

The classic open repair surgical incision adopts a midline approach, but more and more open repairs involve complex intracavitary graft removal, which needs to be based on the intracavitary graft structure, previous abdominal surgery history, retroperitoneal inflammation and the surgeon's preferences. Choose the corresponding approach based on experience. It can take a month or more to fully recover after surgery.
The mortality rate of elective open surgery for abdominal aortic aneurysm is 2% to 8%, and the mortality rate of ruptured abdominal aortic aneurysm surgery in different medical centers at home and abroad is 40% to 70%.
Open abdominal aortic aneurysm repair has certain risks, including massive bleeding, intestinal adhesion, intestinal obstruction, wound non-healing, local infection, etc.In addition, due to the large trauma of surgery, patients recover slowly after surgery, and may suffer complications such as cardiovascular and cerebrovascular accidents and multiple organ failure. Therefore, it is necessary to closely monitor the patient's vital signs and condition changes after surgery,and deal with complications in a timely manner.
EVAR
Eendovascular abdominal aortic repair,EVAR, Due to its minimally invasive, safe and other advantages, it is increasingly used in clinical practice. In recent years, the rapid development of intracavity technology and instruments has promoted the application and promotion of complex EVAR.
At present, most patients can complete the operation under local anesthesia, which significantly reduces surgical trauma and shortens the length of hospital stay. It is especially suitable for patients with severe cardiopulmonary insufficiency and other high-risk factors. At present, the mainstream view in academic circles at home and abroad is that endovascular technology for the treatment of complex abdominal aortic aneurysms has the advantage of low postoperative mortality, while open surgery for the treatment of complex abdominal aortic aneurysms has the advantage of a low recurrence rate.
In addition to the above-mentioned preoperative assessment required for open surgery, EVAR requires detailed assessment of the anatomy of the lesion, and CTA is usually the first choice.The assessment includes the status of the branch arteries and the status of the tumor (including tumor size, shape, mural thrombus, and calcification). and many other indicators. These anatomic factors determine whether a patient is suitable for EVAR and affect postoperative outcomes.
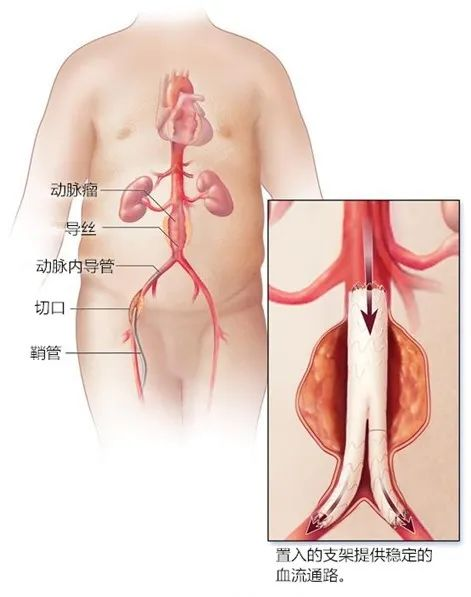
In addition, the contrast agent used during EVAR will increase the burden on the kidneys. When patients with renal insufficiency undergo EVAR, hydration and other measures can be taken before surgery to reduce the risk of contrast agent-related kidney injury. During the operation, the doctor will insert the catheter through the leg artery, then gently guide it to the aorta, and then place the stent at the site of the aneurysm. After releasing it, it will expand and be fixed in place. Stents strengthen weak areas of the aortic wall and prevent aneurysms from rupturing.
In short, endovascular repair of abdominal aortic aneurysm is a safe and effective minimally invasive treatment method, but it also requires strict control of the indications and contraindications, as well as good preoperative preparation and postoperative care.